Wisdom teeth removal is a common dental procedure, often recommended during late adolescence or early adulthood. However, the question often arises: why can’t a general practitioner perform the extraction, and why is an oral surgeon more expensive than other dental specialists? Should wisdom teeth be left alone if they’re not causing any problems? This blog will delve into these questions, providing a comprehensive understanding of the complexities involved in wisdom teeth extractions and the role of an oral surgeon in this process.
The Role of General Practitioners in Dentistry
General practitioners (GPs) in dentistry are akin to primary care doctors in medicine. They are trained to diagnose, treat and manage a broad range of dental issues. A general dentist is your go-to for routine checkups, cleanings, fillings and basic dental care. They are also the first line of defense in diagnosing potential dental problems, including those related to wisdom teeth.
However, when it comes to more complex procedures, such as wisdom tooth extractions, the expertise of an oral surgeon is often required. While some general dentists might perform simple extractions, the extraction of wisdom teeth, especially impacted ones, usually demands a higher level of skill and experience.
Why Can’t a General Practitioner Extract Wisdom Teeth?
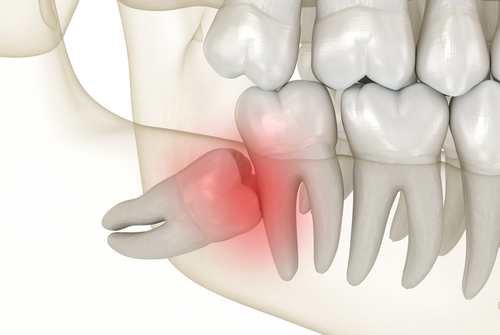
Wisdom teeth, or third molars, are the last set of teeth to emerge, usually between the ages of 17 and 25. Their extraction can be straightforward or complex, depending on several factors such as the position of the teeth, the depth of impaction, and the proximity to nerves and other critical structures. Here’s why general practitioners often refer patients to oral surgeons for wisdom teeth extractions:
- Complexity of the Procedure
Wisdom teeth extractions can range from simple to highly complex. If the wisdom teeth are fully erupted and positioned normally, a general dentist may be able to perform the extraction. However, if the teeth are impacted (meaning they haven’t fully erupted and are trapped within the gum or jawbone), the procedure becomes more complicated. Impacted wisdom teeth can be angled awkwardly, partially covered by gum or bone or situated close to important nerves. These factors increase the risk of complications, making the expertise of an oral surgeon necessary.
- Specialized Training
Oral surgeons undergo additional years of training beyond dental school, focusing on surgical procedures involving the mouth, jaws and face. This specialized training equips them with the skills to handle complex extractions, manage complications and administer sedation. They are also trained to deal with emergencies that may arise during or after surgery, such as excessive bleeding, nerve damage or infections.
- Management of Complications
The removal of wisdom teeth, particularly impacted ones, can sometimes result in complications such as dry socket, infections or damage to nearby teeth or nerves. Oral surgeons are trained to anticipate and manage these complications effectively. Their expertise ensures that any issues are addressed promptly, reducing the risk of long-term damage and improving the overall outcome of the procedure.
- Use of Sedation
Wisdom tooth extractions can be painful and stressful, particularly if the patient is anxious or if the procedure is complex. Oral surgeons are qualified to use a variety of sedation techniques, from local anesthesia to intravenous (IV) sedation and general anesthesia, ensuring that patients remain comfortable and pain-free during the procedure. General dentists may not have the necessary training or equipment to provide these levels of sedation safely.
Why Is an Oral Surgeon Pricier Than Other Dental Specialists?
The cost of wisdom tooth extraction by an oral surgeon can be significantly higher than having the procedure done by a general dentist or another dental specialist. Several factors contribute to this price difference:
- Advanced Training and Expertise
As mentioned earlier, oral surgeons undergo additional years of education and training. This specialized knowledge and skill set justify higher fees, as patients are paying for the surgeon’s expertise in managing complex cases and minimizing the risk of complications.
- Higher Level of Care
Oral surgeons often handle cases that require a higher level of care, such as impacted wisdom teeth, teeth close to nerves or teeth associated with cysts or tumors. The equipment, techniques and care involved in these procedures are more sophisticated, which increases the overall cost.
- Comprehensive Pre- and Post-Operative Care
The cost of seeing an oral surgeon typically includes not just the procedure itself, but also the comprehensive care provided before and after surgery. This includes pre-operative consultations, imaging (such as X-rays or CT scans), sedation, the procedure itself and follow-up appointments to ensure proper healing. This level of care is critical in managing potential complications and ensuring a successful outcome.
- Use of Advanced Technology
Oral surgeons often use advanced imaging technology, such as 3D cone beam CT scans, to plan and execute the extraction with precision. This technology is costly but provides detailed information about the patient’s anatomy, which is crucial for avoiding complications and ensuring a safe extraction.
Should Wisdom Teeth Be Left Alone?
One of the most common questions patients have is whether wisdom teeth should be removed if they aren’t causing any pain or problems. The answer isn’t always straightforward, as it depends on several factors:
- Impacted Wisdom Teeth
Impacted wisdom teeth are those that have not fully erupted and are stuck in the jawbone or under the gum tissue. Even if they are not causing immediate pain, impacted wisdom teeth can lead to problems over time, such as infections, cysts or damage to adjacent teeth. In these cases, removal is often recommended to prevent future complications.
- Risk of Future Problems
Even if wisdom teeth are not currently causing problems, they may pose a risk for future issues, particularly if they are difficult to clean. Wisdom teeth are located at the back of the mouth, making them harder to reach with a toothbrush and floss. This can lead to cavities, gum disease and infections. In some cases, proactive removal of wisdom teeth is recommended to avoid these potential issues.
- Age and Oral Health
The decision to remove wisdom teeth may also depend on the patient’s age and overall oral health. Younger patients tend to recover more quickly from extractions, and the procedure is generally easier when the teeth are still developing. For older patients, the extraction can be more challenging, and the recovery process may be longer. If a patient has poor oral health or is at risk for complications, an oral surgeon may recommend removal even if the wisdom teeth are not currently causing problems.
When Do I Need to Get Wisdom Teeth Removed?
The decision to remove wisdom teeth is based on a thorough evaluation by a dentist or oral surgeon. Here are some scenarios where wisdom teeth removal is typically recommended:
- Pain and Discomfort
If you’re experiencing pain or discomfort in the back of your mouth, it could be a sign that your wisdom teeth are coming in or are impacted. Pain may be constant or occur only when chewing or brushing. In such cases, an evaluation is necessary to determine if extraction is needed.
- Infection or Gum Disease
Partially erupted wisdom teeth can create a flap of gum tissue that traps food and bacteria, leading to infections. Symptoms of infection include pain, swelling, redness and bad breath. Gum disease around wisdom teeth is also common and can spread to adjacent teeth if not treated.
- Crowding and Misalignment
If your wisdom teeth are growing in at an angle or there’s not enough room in your mouth, they can push against other teeth, causing crowding and misalignment. This can undo years of orthodontic work and lead to a less attractive smile. In such cases, removal is recommended to preserve the alignment of your teeth.
- Cysts and Tumors
In rare cases, impacted wisdom teeth can lead to the formation of cysts or tumors in the jawbone. These growths can cause significant damage to the jaw and surrounding teeth, requiring more extensive surgery to remove. Regular dental checkups and X-rays can help detect these issues early, often leading to the recommendation for extraction.
- Difficulty Cleaning
Even if your wisdom teeth have fully erupted and are not causing pain, they can be difficult to clean due to their location at the back of the mouth. This can lead to cavities, gum disease and other dental problems. If your dentist notices signs of decay or gum issues, they may recommend extraction to prevent further complications.
What Happens If I Leave Wisdom Teeth Alone?
If you choose not to have your wisdom teeth removed, it’s essential to understand the potential risks and complications that could arise. While some people never experience problems with their wisdom teeth, others may face significant issues over time.
- Increased Risk of Infection
Partially erupted or impacted wisdom teeth create an environment where bacteria can thrive, leading to infections. These infections can be painful and may require antibiotics or, in severe cases, emergency surgery. Recurrent infections are a strong indicator that wisdom teeth should be removed.
- Damage to Adjacent Teeth
Impacted wisdom teeth can press against the neighboring molars, causing damage to the enamel and increasing the risk of cavities. Over time, this pressure can lead to decay or even fracture of the adjacent teeth, potentially requiring additional dental work such as fillings, crowns or even extractions.
- Development of Cysts or Tumors
As mentioned earlier, leaving impacted wisdom teeth in place can sometimes lead to the development of cysts or tumors. These growths can cause bone loss and damage to nearby teeth, requiring more invasive surgery to correct.
- Crowding and Misalignment
Wisdom teeth that grow in improperly can cause your other teeth to shift, leading to crowding and misalignment. This can be particularly problematic for individuals who have previously undergone orthodontic treatment, as it can undo the results and necessitate further treatment.
- Chronic Discomfort
Even if your wisdom teeth aren’t causing severe pain, they can still lead to chronic discomfort over time. This can manifest as pressure, headaches or a dull ache in the jaw, which can be bothersome and affect your daily activities. Over time, what starts as mild discomfort can escalate into more serious pain, requiring intervention.
Why Early Removal of Wisdom Teeth Is Often Recommended
Given the potential complications associated with leaving wisdom teeth alone, many dental professionals advocate for their early removal. This recommendation is based on several key factors:
- Easier Recovery in Younger Patients
Younger patients typically recover more quickly and with fewer complications than older adults. The roots of the wisdom teeth are not fully developed in younger individuals, and the surrounding bone is less dense, making the extraction process easier. Additionally, younger patients tend to heal faster, with a lower risk of complications such as dry socket.
- Prevention of Future Problems
Removing wisdom teeth before they cause problems can prevent the development of painful and costly dental issues down the road. Proactive removal helps avoid infections, cysts and damage to adjacent teeth. It also prevents the potential for wisdom teeth to disrupt orthodontic work or cause crowding.
- Better Oral Health Outcomes
By removing wisdom teeth early, you can maintain better overall oral health. Wisdom teeth are difficult to clean, and their presence can make it harder to keep your mouth free of plaque and bacteria. Early removal can help preserve the health of your remaining teeth and gums, reducing the likelihood of cavities and gum disease.
The Procedure and Recovery: What to Expect
If your oral surgeon recommends wisdom tooth extraction, it’s essential to know what to expect before, during and after the procedure.
- Pre-Operative Evaluation
Before the extraction, your oral surgeon will conduct a thorough evaluation, which may include X-rays or a 3D scan to assess the position of your wisdom teeth and their relationship to surrounding structures. This helps the surgeon plan the procedure and anticipate any potential challenges.
- The Extraction Process
On the day of the surgery, you’ll be given anesthesia to ensure comfort during the procedure. The type of anesthesia used will depend on the complexity of the extraction and your level of anxiety. Options include local anesthesia, IV sedation or general anesthesia.
The oral surgeon will then make an incision in the gum tissue to expose the tooth and bone. In some cases, the tooth may need to be divided into sections for easier removal. Once the tooth is extracted, the site is cleaned, and stitches may be placed to aid healing.
- Post-Operative Care
After the procedure, you’ll be given detailed instructions on how to care for the extraction site. This includes managing pain with prescribed medications, using ice packs to reduce swelling, and following a soft diet for the first few days. It’s crucial to avoid smoking, drinking through a straw or any activity that could dislodge the blood clot from the extraction site, as this can lead to dry socket, a painful condition that delays healing.
Most patients experience some swelling and discomfort for a few days after the extraction, but these symptoms typically subside within a week. Your oral surgeon will schedule a follow-up appointment to ensure that the healing process is progressing as expected.
Conclusion
Wisdom tooth extraction is a significant procedure that often requires the expertise of an oral surgeon, especially when dealing with impacted or complicated cases. While general practitioners can handle simple extractions, the complexity of wisdom teeth often necessitates a higher level of skill and experience that only an oral surgeon can provide. The cost associated with seeing an oral surgeon is reflective of their advanced training, the complexity of the procedure and the comprehensive care they provide.
Deciding whether to remove wisdom teeth or leave them alone depends on various factors, including the potential for future problems, the current state of your oral health and the recommendation of your dentist or oral surgeon. While some individuals may never experience issues with their wisdom teeth, the risks associated with leaving them untreated—such as infections, damage to adjacent teeth and the development of cysts—often make proactive removal the best course of action.
If you are considering whether to have your wisdom teeth removed, consult with your dentist or an oral surgeon to discuss your specific situation. Their expert advice, based on a thorough evaluation of your oral health, will help you make an informed decision that ensures the long-term health and comfort of your smile.
